Why severely affected stroke patients deserve more (options, time, hope)
- Leonardo Boccuni
- Aug 10, 2022
- 6 min read
In 2015 McCabe et al. published the results of an extensive, motor learning-based randomized controlled trial targeting severely affected patients in the chronic phase post stroke. By reading the original article or watching the supplementary video (here below) you will get a glance of the meaningful functional gains that could be achieved with severely affected patients, when ambitious interventions are provided.
Unfortunately, there are two vicious cycles that limit the potential for recovery in case of severe hemiplegia. The first one is the inability to accomplish a functional task without external help (therapist and/or assistive devices) limiting the amount of training performed, which in turn hampers motor re-learning. The second mechanism is more insidious and is related to patient's and therapist's negative expectations: in short, severely affected patients have poor recovery prognosis, which could be interpreted by thinking that there is no possibility for recovery; the likely consequence of this belief is the provision of less therapy for the affected arm, thus resulting in a self-fulfilling prophecy.
In contrast with this tendency, evidence is consistently showing that severely affected patients can achieve clinically meaningful improvements; the common ground of successful interventions is breaking the two vicious cycles of insufficient motor training and negative expectations.
To facilitate the translation of research findings into clinical practice, in this article we will briefly outline three concepts:
Part 1. Therapeutic options
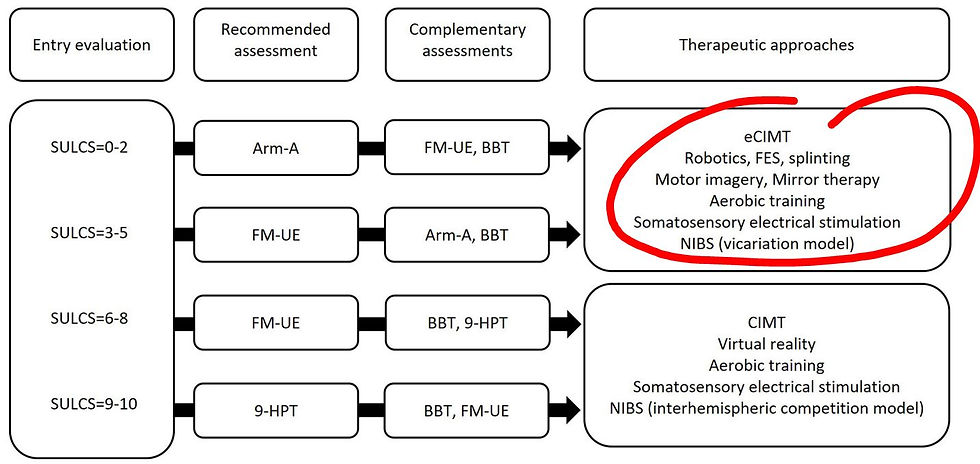
In a recent article we pointed out 10 interventions that fit bests with severely affected patients:
Expanded Constraint Induced Movement Therapy (e-CIMT, a novel version of CIMT adapted to severe hemiplegia)
Cross Training
Robotics
Functional hand splinting
Functional electrical stimulation
Action observation
Motor imagery
Mirror therapy
Somatosensory electrical stimulation
Neuromodulation (based on vicariation model)
Let's briefly summarize keypoints of these interventions:
1. E-CIMT considers high amount of therapy to promote active use of the affected limb, similarly to the original CIMT version. However, the triad of preparatory manipulations to reduce muscle tone, bilateral arm training and use of assistive devices is here applied systematically, to take into account patient's needs and capabilities. Patients indeed recovered to a considerable extent when undertaking e-CIMT, which was not the case with conventional therapy.

2. Cross training consists on systematic motor practice of the unaffected limb, because functional gains that transfer to the affected limb have been observed. There are two types of training to consider: fine skill training (gaming/sport/music alike) challenging the unaffected arm to the limit of patient's capabilities; and strength training, because it may trigger bilateral pathways (such as the reticulospinal tract) responsible for force production and potential neural basis for recovery (see later).
3. 4. 5. Assistive devices should be used to train whole-arm functional tasks, such as reaching and grasping. Robotics assist shoulder and elbow movements, by providing guidance and anti-gravity support; splinting helps stabilizing the wrist and recreating a palmar concavity; functional electrical stimulation produces active-assisted muscle contraction, particularly useful for finger extension.
6. 7. 8. Action observation, motor imagery and mirror therapy are ways of accessing cortical sensorimotor networks even in the absence of any movement. They should be considered as preparatory interventions immediately before the formal motor training session.
9. Somatosensory electrical stimulation is another intervention to prime neuroplasticity through the sensorimotor connection, can be easily implemented and applied by the patient independently in the two hours preceding motor training.
10. Finally, neuromodulation priming alternative pathways (premotor ipsilateral and contralateral CST) should be considered because of the cooperative (and not competitive) role of these pathways for severely affected patients. In particular, spaced neuromodulation is a promising novel field of neuromodulation.
Part 2. Amount of therapy
A cornerstone element to be considered is the amount (time, repetitions) of therapy delivered. Mildly impaired patients will recover faster because of relatively preserved integrity of the corticospinal tract, but also because they can perform enough motor training within the formal therapy session, and also practice indipendently throughout the day. On the other hand, severely affected patients would recover to a certain extent through alternative pathways, and they have to rely on external assistance and adaptations to train functional activities; so it is pivotal to guarantee enough therapy for these patients. To make an approximate estimate, three hours a day could be considered the threshold to guarantee functional gains.
Coming back to the article of McCabe et al., patients with severe chronic stroke were divided in three groups that received the same amount of therapy (five hours a day, five days a week, 12 weeks), differing for the provision of motor learning training in one group, robotics in another, and FES in the third group. All three groups improved far beyond the minimally clinical meaningful change, without any between-group differences; which is an excellent example of the importance of providing adequate amount of therapy, irrespective of the specific treatment modality.

However, the vast majority of rehabilitation facilities cannot guarantee this amount of therapy, and patients cannot usually cover the costs of daily therapy sessions. Furthermore, it has been demonstrated that distributing motor practice in several practice sessions is better than undertaking all motor training in one session. Taken together, it's clear that we should find strategies to allow patients to train without the constant presence of a therapist, for instance by using assistive devices, or to plan group sessions that makes treatments economically sustainable.
Here the take home message is to work intensively with your patient during therapy to maximize the impact of the intervention, and then explore solutions to allow patients to train unassisted or unsupervised.
One final note about amount of therapy: time after stroke matters. While it is true that in the chronic phase, the more the better, in the acute phase after stroke caution should be taken to avoid overloading the therapy dosage; in fact, very early intensive interventions have shown better outcomes for those patients undertaking lower dosages and a distributed schedule, as compared to higher dosages concentrated in one big session.

Part 3. Neural basis for recovery
For severely affected patients, it is likely that corticospinal tract integrity have been compromised to the point that recovery cannot rely on the reactivation of the original primary sensorimotor areas. Nonetheless, functional reorganization is possible by targeting alternative cortical and subcortical resources. To summarize, at the cortical level we could improve the activation of premotor areas, such as the supplementary motor area (task sequence), premotor dorsal area (goal oriented actions for reaching a target) and the premotor ventral area (hand shaping for effective grip). The pathways originating from these areas account for one third of the overall corticospinal tract and have more bilateral transcallosal and cortico-reticular connections, as compared to fibres originating from the primary motor area.

Furthermore, the controlateral hemisphere can connect with ipsilateral spinal motorneurons, directly or indirectly through the pontomedullay reticular formation. At this point, it's worth consider the potential role of reticular formation in functional recovery. To make a practical example, let's consider a selective hand movement, like finger tapping, which involves the activation of the primary motor area; by contrast, a whole-hand strong grasping requires the activation of the reticular formation. In fact, reticular formation is capable of generating high amount of forces, but not to generate fine movements. Therefore, training severely impaired patients may result in the recovery of grasping movements, but not finger individuation. Put simply, you can recover the ability to pick up a bottle and drink from it, not to play the piano.

To summarize, knowing the neural basis helps us understand clinical deficits and recovery; from one hand, it is encouraging that the brain is capable of reorganize itself, given that adequate training is provided; from the other hand, we have to acknowledge the limits of recovery in order to have an optimistic, yet balanced attitude when it comes to goal setting.
I would like to conclude this article with a brief consideration, that escapes from the rigour of scientific research and quantitative results. We (clinicians) are dealing with people (patients), not an arm, a leg or a trunk, and not even a brain. Helping patients to recover from a sudden and catastrophic event such as a severe stroke inevitably involves emotions on both sides. That is to say that, irrespective of the final objective outcome that we may achieve, patients are experiencing unconditioned help from a therapist, working to the very best of his/her capabilities and always keeping a positive attitude. This positive feeling of being truly supported is everlasting, and we should consider it to conclude that, after all, it's always worth the effort.






Hola Leonardo
Muy interesante el artículo! Además de las fuente que son muy útiles. Oye, que dispositivo de antigravedad para la extremidad superior empleas en el vídeo?